Diabetes is a disease that affects blood vessels throughout the body, particularly vessels in the kidneys and eyes. When the blood vessels in the eyes are affected, this is called diabetic retinopathy.
The retina is a light-sensitive tissue at the back of the eye. When light enters the eye, the retina changes the light into nerve signals. The retina then sends these signals along the optic nerve to the brain. Without a retina, the eye cannot communicate with the brain, making vision impossible.
Major blood vessels lie on the front portion of the retina, and when these blood vessels are damaged due to diabetes, they may leak fluid and lipids (fats) and grow scar tissue. This leakage, called macular edema, affects the ability of the retina to detect and transmit images. Left unchecked, this may eventually lead to glaucoma, or cataracts, or a complete destruction of the retina, and even eventual blindness.
There are two types of diabetic retinopathy:
Also known as background retinopathy, this is an early stage of diabetic retinopathy and occurs when the tiny blood vessels of the retina are damaged and begin to bleed or leak fluid into the retina resulting in swelling (diabetic macular edema) and the formation of deposits known as exudates. Many people with diabetes develop mild NPDR often without any visual symptoms.
This carries the greatest risk of loss of vision and typically develops in eyes with advanced NPDR. PDR occurs when blood vessels on the retina or optic nerve become blocked consequently starving the retina of necessary nutrients. In response, the retina grows more blood vessels (neovascularization). Unfortunately these new vessels are abnormal and cannot replenish the retina with normal blood flow. PDR may lead to any one of the following:
Diabetic retinopathy often has no early warning signs. During the early stages of diabetic retinopathy, reading vision is typically not affected. However, when retinopathy becomes advanced, tiny blood vessels grow along the retina, in the clear, gel-like vitreous humor that fills the inside of the eye.
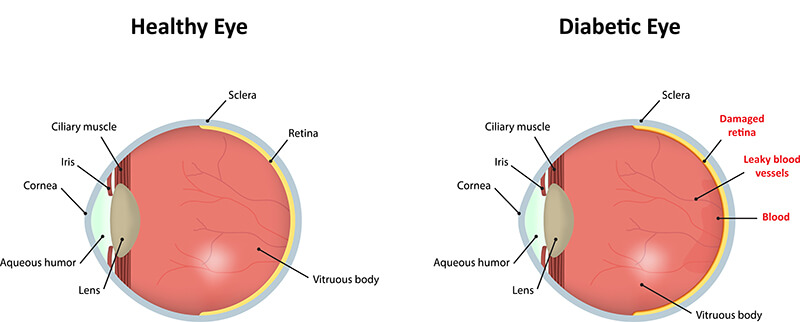
These vessels are the body’s attempt to overcome and replace the ones that have been damaged by diabetes. However, these new vessels are thinner and weaker than normal and may bleed into the vitreous humor, clouding vision. Usually, the first few times this happens, tiny spots of blood are left floating in the way of vision, often dissipating after a few hours.
Within a few days or weeks, these spots can be followed by a much greater leakage of blood, which tend to happen more than once, often during sleep. Vision may become completely blurred and may take anywhere from a few days to months or even years to clear. In extreme cases, the blood does not clear and the only vision remaining is the ability to differentiate light from darkness.
Things Dr. Seibel will look for and ask you about:
All people with diabetes are at risk – those with Type I diabetes (juvenile onset) and those with Type II diabetes (adult onset).
Although, everyone who has diabetes is at risk for developing diabetic retinopathy, not everyone develops it. Generally, diabetics don’t develop diabetic retinopathy until they’ve had diabetes for at least 10 years. Changes in blood sugar levels increase the risk.
Women with diabetes have a slightly higher risk during pregnancy. It is recommended that all pregnant women with diabetes have dilated eye examinations each trimester to protect their vision.
A dilated eye exam is the only way to detect changes inside the eye before loss of vision begins. People with diabetes should have an eye examination at least once a year. More frequent exams may be necessary after diabetic retinopathy is diagnosed.
Treatments are very effective in reducing vision loss from this disease. In fact, even people with advanced retinopathy have at least a 90 percent chance of keeping their vision if they get treatment before the retina is severely damaged. Treatments include:
Laser treatments are available for:
A procedure called scatter laser treatment dissolves the abnormal blood vessels that form at the back of the eye. Rather than focusing on a single spot, hundreds of tiny laser zaps shrink the abnormal blood vessels from the center of the retina. Side vision is typically affected by this treatment in order to save the remaining central sight and may need repeating if new blood vessels appear.
This laser surgery, called focal laser treatment, if performed early enough can reduce vision loss from macular edema by half. During the surgery, a high-energy beam of light is aimed directly onto the damaged blood vessels. It seals the vessels and stops them from leaking. Sometimes, more than one treatment may be needed to completely control the leaking fluid.
Instead of laser surgery, an eye operation called a vitrectomy may be needed to restore sight. A vitrectomy is performed in cases that have a lot of blood in the vitreous. It involves removing the cloudy vitreous and replacing it with a special salt solution.
At Seibel Vision Surgery, your eyes and vision are of paramount importance. To help you make the most informed decisions regarding the welfare of your vision, we are delighted to be of service and are happy to answer any questions you may have.
Please take the time to familiarize yourself with the information contained on this site. We have compiled it especially for you!
Monday, Tuesday, Wednesday, and Thursday
8:30 a.m. to 3:30 p.m.
Friday
8:30 a.m. to 3:00 p.m.
OUR ADDRESS
11620 Wilshire Boulevard, Suite 711
Los Angeles, California 90025
PHONE
(310) 444-1134
FAX
(310) 444-1130
Learn about cataracts and their treatment
Learn more about CataractsGlaucoma, Macular Degeneration,
Medical Eye Exams, and other