If you have been diagnosed with age-related macular degeneration (ARMD) you are in very good company. In the United States alone, a new case is diagnosed every three minutes:
Although it almost never causes total blindness, macular degeneration is the leading cause of vision loss in people over 50 in our country. Work with your doctor to learn to identify the problem early in an attempt to keep it from getting worse or to slow it down.
Macular degeneration is a disease caused by damage or the breakdown of the macula, a tiny oval area in the retina, where the photoreceptors are most dense and where incoming images are focused.
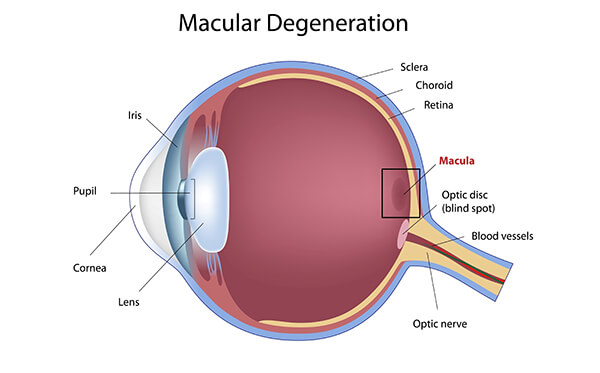
The center of the macula is called the fovea and is responsible for fine detail vision – our central (or reading) vision, both for distance and close up. When the eye is directed at an object to be seen, whichever part is focused on the fovea will be the clearest, the most in-focus image seen. So, your ability to see fine centralized detail is directly dependent upon the condition of the macula and fovea.
In macular degeneration, something goes wrong with the macula (as explained in more detail below) and it slowly stops working. When this happens, vision fades in the middle (the fovea), usually leaving the peripheral, or side vision. It is uncommon for someone with macular degeneration to lose both macular (detail) and peripheral (side) vision, or to lose vision completely in both eyes.
There are two forms of age-related macular degeneration:
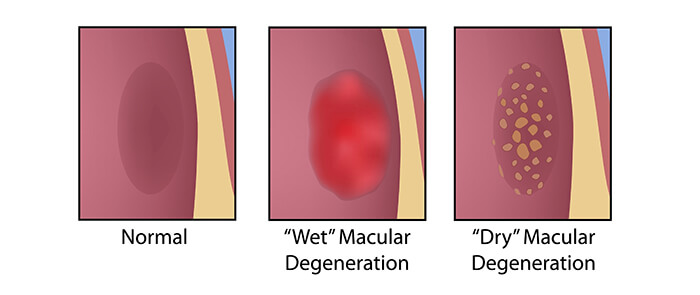
The vast majority of cases of ARMD are the dry type, which always precedes the wet type, although it doesn’t always turn into that. Dry refers to the slow degenerative process that occurs in which the macula forms yellow deposits, called drusen and then becomes progressively thinner but does not leak, and so is considered ‘dry’.
Progression of dry macular degeneration takes a very long time and does not always affect both eyes equally. Most people usually maintain some central vision in at least one eye.
Wet ARMD always arises from pre-existing dry ARMD. This occurs in about 10 to 15% of people with advanced dry macular degeneration. Newly formed, abnormal blood vessels grow underneath the retina in the area of the macula. These vessels leak fluid, bleed, and lift up the retina. When this happens central vision is reduced and is often distorted. Eventually, scar-like tissue forms under the macula and the eye loses its ability to see detail. If CNV occurs in one eye, there is an increased chance it will occur in the other eye.
There is no pain associated with dry or wet macular degeneration. Vision loss usually occurs gradually and typically affects both eyes at different rates. Sometimes only one eye loses vision while the other eye continues to see well for years. If both eyes are affected, reading and close up work can become quite difficult. Even with a loss of central vision, however, peripheral vision may remain clear.
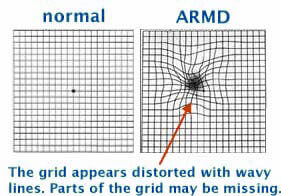 The condition may be hardly noticeable in its early stages. A very frequent and important symptom to be aware of is distortion. Straight lines will not look straight. A telephone pole or a door frame may seem a little bent, crooked, or irregular, as though seen through heat waves on a highway. An area of the Amsler grid will appear distorted and the small boxes in the area will vary in shape and size. Also, you may see a dark gray spot similar to the aftereffect caused by a flashbulb. There may be other changes in vision: you may notice that the size of an object appears different for each eye or that colors don’t look the same for each eye. These changes in eyesight are important symptoms and anyone who has these symptoms should make sure to see the eye doctor promptly.
The condition may be hardly noticeable in its early stages. A very frequent and important symptom to be aware of is distortion. Straight lines will not look straight. A telephone pole or a door frame may seem a little bent, crooked, or irregular, as though seen through heat waves on a highway. An area of the Amsler grid will appear distorted and the small boxes in the area will vary in shape and size. Also, you may see a dark gray spot similar to the aftereffect caused by a flashbulb. There may be other changes in vision: you may notice that the size of an object appears different for each eye or that colors don’t look the same for each eye. These changes in eyesight are important symptoms and anyone who has these symptoms should make sure to see the eye doctor promptly.
Do not assume you simple need a new pair of glasses. Make your appointment right away.
The root causes of macular degeneration are unknown. Women are at a slightly higher risk than men. Caucasians are more likely to develop macular degeneration than African-Americans.
The macular contains many highly active and sensitive photoreceptors that require and consume a great deal of energy. Generating this energy requires a constant, rich supply of oxygen, nutrients and ions. Consequently, the macula has one of the highest volumes of blood flow through its supply vessels. Anything that interferes with this necessary rich blood supply can cause the macula to malfunction and possibly become diseased.
Smoking is one of those factors that can reduce this vital blood supply by contributing to overall narrowing of the blood vessels and thickening of the blood. A high-fat, high cholesterol diet can lead to fatty plaque deposition in the macular vessels, also hampering blood flow. Nutritional deficiencies, such as shortage of antioxidants, may increase the tendency for fatty deposits to stick to blood vessel walls.
In order to determine if you have macular degeneration and what form, your doctor will measure your vision and examine your eyes. By looking at the retina, your doctor will be able to tell if there is an abnormality. If drusen are found, you will want to schedule regular check-ups to make sure that no further damage is occurring. It may be necessary that photographs of each macula be taken to use for future comparison.
The following are tests given to fully diagnose AMD:
Regardless of the treatment therapy followed, patients with advanced dry macular degeneration should check the vision in each eye, one at a time, at least once a day by staring at the central point on an Amsler grid.
We have provided a printable Amsler grid and instructions for use for you. Patients can help monitor their vision regularly and can detect distortions in vision. These distortions represent the earliest stages of wet macular degeneration.
In the early stages of dry macular degeneration, regular eye check-ups, attention to diet, in-home monitoring of vision and possibly nutritional supplements may be all that is recommended.
Currently, treatments for macular degeneration are rapidly advancing and changing as often as every three months. Various treatments are currently available, but most of these treatments are directed at the early stages of wet ARMD.
For those patients with wet AMD, there is significant hope in the very near future. Ongoing clinical research is investigating new treatment strategies using photodynamic therapy. These studies are underway and the preliminary results are very encouraging.
One recent strategy that seems promising is a new class of drugs known as anti-angiogenic agents, which may stop the formation of blood vessels in wet AMD and cause existing abnormal vessels to regress.
The names of these drugs are rhuFab V2 (Genentech, Inc.), Macugen (Eyetech Pharmaceuticals) and Anecortave acetate (Alcon Research Ltd.). The preliminary results are encouraging, however these drugs are only available at this time to patients participating in a clinical study.
For those patients who have already experienced vision loss and are somewhat stable, there is a new low vision device that is undergoing clinical investigation. This device is known as an intraocular miniature telescope (IMT) and is inserted into the eye at the time of cataract surgery. While this device may not help all patients with AMD, there is a very good chance that the IMT could improve the ability to read and watch television.
All treatments, so far, are designed to treat the vision loss associated with wet AMD and slow the progression of the disease. None of the therapies really treat the underlying cause of AMD. While the cause is still unknown, there is solid evidence that this is a disease with a strong genetic basis. For this reason, a great deal of research is going on to find the genes responsible for AMD in the hope of someday developing a cure.
At Seibel Vision Surgery, your eyes and vision are of paramount importance. To help you make the most informed decisions regarding the welfare of your vision, we are delighted to be of service and are happy to answer any questions you may have.
Please take the time to familiarize yourself with the information contained on this site. We have compiled it especially for you!
Monday, Tuesday, Wednesday, and Thursday
8:30 a.m. to 3:30 p.m.
Friday
8:30 a.m. to 3:00 p.m.
OUR ADDRESS
11620 Wilshire Boulevard, Suite 711
Los Angeles, California 90025
PHONE
(310) 444-1134
FAX
(310) 444-1130
Learn about cataracts and their treatment
Learn more about CataractsGlaucoma, Macular Degeneration,
Medical Eye Exams, and other